Are you still struggling with hip pain after delivering your baby weeks, months, or decades ago?
Well, don’t worry. You’re not alone. Postpartum joint pain is widespread among women after childbirth.
In pregnancy, reports suggest that up to 25% of women experience serious pain– with 8% reporting severe disability. But many women suffer from disabling hip and joint pain long after giving birth to their babies.
These post-delivery joint pains may be pains that start during your pregnancy or new pains that begin during or shortly after the birth. The pains also manifest in several different ways.
From hip pain and pelvic girdle pain caused by the pregnancy and/or the delivery. Pain in the finger joints due to increased fluid retention or knee pain that occurs because your knees support the additional weight of your baby.
But the most common cause of pre and postpartum joint pain is hip pain, which develops during the pregnancy and can continue for weeks or months after the delivery.
Postpartum hip pain can become chronic and long-lasting in rare cases (without proper treatment).
All these complaints are likely due to inflammation and physical changes during pregnancy, childbirth and post-partum. They can also occur due to hormonal changes.
More Blogs From Focus Osteopathy
How Pregnancy Can Cause Knee And Back Pain
When your shoulder is really a pain in the neck…
How does our modern lifestyle affect posture?
What Are The Symptoms Of Hip Pain After Pregnancy?

Medically, we refer to pain around the area that we call our “hips” – as Pelvic Girdle Pain (PGP) because it usually affects the pelvic joints.
Pain patterns tend to differ between women, but the main symptoms of PGP are:
- Your hips feel “loose” – sometimes, this might feel like all the muscles around the hips are stiff and tight, but your pelvis feels unstable.
- Intense pain in the hips, deep inside your pubic region, your legs, lower back, or butt.
- A loud popping sound when you move your hips
- Pain that radiates over the lower back
- Pain that worsens with activity
Your doctor may prescribe pain medication to deal with the pain. Still, longer-term physical therapy, specifically in the form of osteopathy and therapeutic exercise, is recommended to treat the root cause, strengthen the weakened pelvic floor muscles, and lessen the pain – without resorting to pain pills.
What Causes Hip Pain After Pregnancy?
There isn’t one main reason why hip or pelvic girdle pain occurs during and after pregnancy.
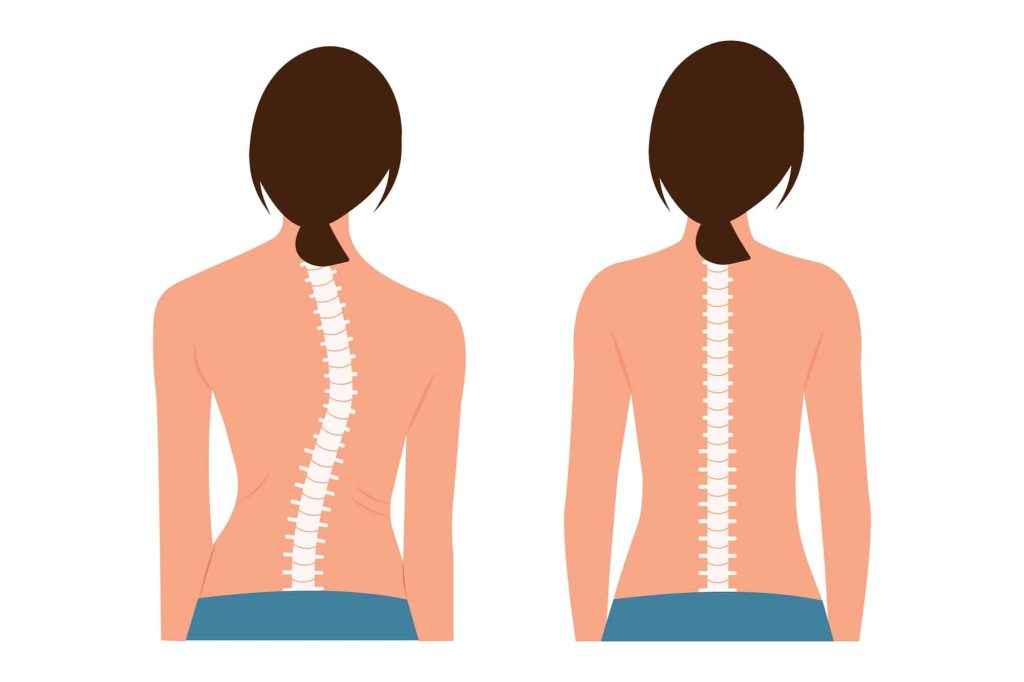
Still, in most cases, the cause usually relates to how pregnancy results in changes to the body’s posture, ligaments, muscles and support structures.
Why? Because the hormones our bodies release during pregnancy stretch specific ligaments and tendons, which can cause pelvic girdle pain and pain in the hips.
The pelvic girdle plays a pivotal role in connecting your upper and lower body. Hence, there is pressure and stress on the hips and pelvic girdle every time you move.
In addition, numerous muscles are running through or connecting to the hips and pelvic girdle.
These include the psoas, the hamstrings, the glutes, and your all-important pelvic floor muscles.
As a result, many things can go wrong and cause pain in the “hip” area – especially when everything is extra stretchy and flexible.
Interestingly, hormones can also affect our pain regulation, so your perception of the intensity of the pain may be greater than before you got pregnant.
But what causes the pain?

Well, the precise cause of PGP and hip pain after pregnancy is different for everyone, so you need to book in for a complete evaluation.
But for information purposes, here are causes of “hip” pain that may linger after pregnancy:
- Piriformis syndrome: This painful syndrome occurs when the piriformis muscle close to the buttocks gets spasms, leading to pain.
In some cases, piriformis syndrome can also irritate the sciatic nerve and cause it to flare up, leading to sciatica – during and after pregnancy.
Sciatica causes nerve pain in the leg, hip, and lower back. However, with physical therapy, most women can successfully manage the symptoms of piriformis syndrome and/or sciatica and relieve the pain without pain pills. - Labral tears: This issue is common during labour and childbirth – when the labrum (cartilage) inside the hip socket suffers damage and tears.
But if this were the cause of your hip pain, you would probably know about it at the time because the pain can be excruciating and make walking difficult.
However, doctors can miss small tears, so we recommend you get an evaluation of your hips to check whether this is the case for you. - Arthritis: Certainly, with osteoarthritis, pregnancy is unlikely to be the cause of arthritis, but unfortunately, in some cases, pregnancy is the catalyst for a flare-up of arthritic symptoms that alert you and your doctor to this underlying medical condition.
But osteoarthritis is more common in older postmenopausal women, so this is unlikely to be the case for you.
However, in the case of rheumatoid arthritis, some women develop this condition after giving birth because the immune system begins to attack joint tissues. But this is rare.
Both types of arthritis are chronic, lifelong conditions. Still, osteopathy and physical therapy can reduce the intensity of the symptoms and prevent further progression. - Pelvic bone problems: As your baby moves through the birth canal, they can bruise or fracture your pelvic bones and cause pain that lingers after pregnancy.
Especially if labour is fast, pain from bruising will subside in most cases, but you may need an X-ray to check for fractures if it continues. - Symphysis pubis dysfunction refers to the pain that occurs when your left and right pelvic bones move and separate to accommodate your growing baby.
This type of pain is primarily felt in pregnancy. It should go away after pregnancy, but you may feel additional pain. At the same time, your bones move back to their pre-pregnancy position. - Hyperthyroidism: In most cases, hyperthyroidism is unlikely to be the cause of your hip pain, but due to the increased demand for your thyroid gland, many women do suffer from hyperthyroidism when pregnant.
This condition occurs when the thyroid gland secretes excessive hormones. In many cases, this secretion is due to an underlying condition called Grave’s Disease.
But for the one in four women that develop this condition for the first time during pregnancy, the symptoms can get more severe after delivery. In addition, during and after pregnancy, women who suffer from hyperthyroidism during and after pregnancy can sometimes develop thyrotoxic myopathy.
This disorder can impact the pelvic girdle leading to pain in the area. But the good news is that your doctor can run tests to determine whether you have this condition.
They can also prescribe antithyroid medicines to help you maintain normal thyroid levels and alleviate joint pain symptoms.
How To Reduce Hip Pain After Pregnancy

There are many causes of hip and joint pain after giving birth. While some are common and not too serious, others might pose health issues and require treatment.
If your joint pain continues more than a month after the pregnancy or the pain increases, it is essential to consult a doctor, osteopath, or physical therapist.
At Focus Osteopathy, we are highly experienced in pregnancy and postnatal pain and recovery and we can support you throughout your pregnancy journey.
Pregnancy can take a toll on your body, especially if you’re ill-prepared and don’t have osteopathy or physical therapy to prepare for the birth.
Unfortunately, there is no quick fix. But you can recover much faster when you know the root cause of your pain and have a natural recovery plan tailored to your specific set of symptoms.
We get to the core of your postpartum pain and help you feel better quickly. Book your free consultation now.
If your hip pain after pregnancy is mild, there are some ways you can treat the pain at home. For example, if you have pain in your lower back, you can try alternating hot/cold compressed to relieve the pain.
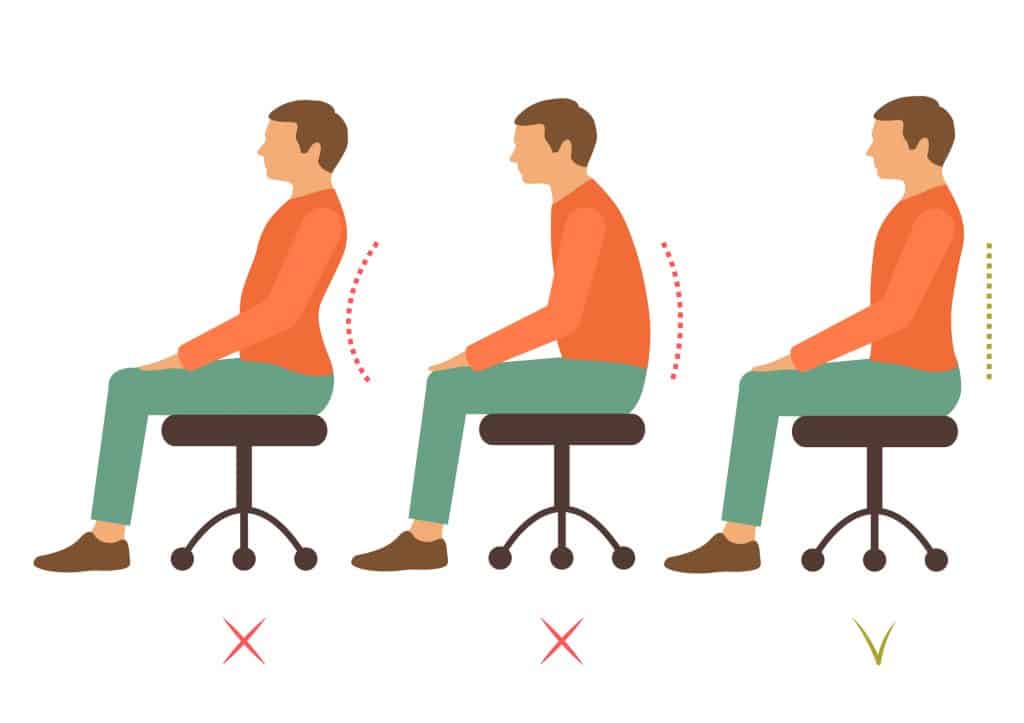
However, we know that hip pain can often result from poor posture or an incorrect gait (walking pattern) that places stress on your hip joints and leads to pain, which we can help you with at the clinic.
But here are a few ways you can prevent hip pain at home:
- Do stretching exercises (preferable exercises provided by us)
- Eat well and increase your intake of lean protein, fresh vegetables, and fruit
- Reduce your caffeine intake
- Do daily exercise to strengthen weak muscles (preferable exercises provided by us: walking, Pilates, Yoga – or resistance training if you’re cleared to)
- Wear the right kind of footwear
- Maintain a healthy weight
- Make sure you get adequate calcium and vitamin D
- Lead a physically active lifestyle
However, even if your pain is mild, we would still recommend that you book a consultation to check that nothing is going on that might get worse with time.
It’s Time To Take Action

Hip pain is common and you shouldn’t have to suffer in silence.
Reaching out is the first part of the recovery process.
If any of this sounds familiar to you don’t hesitate to get in touch.
We know that we can help you set up a personalized recovery plan.