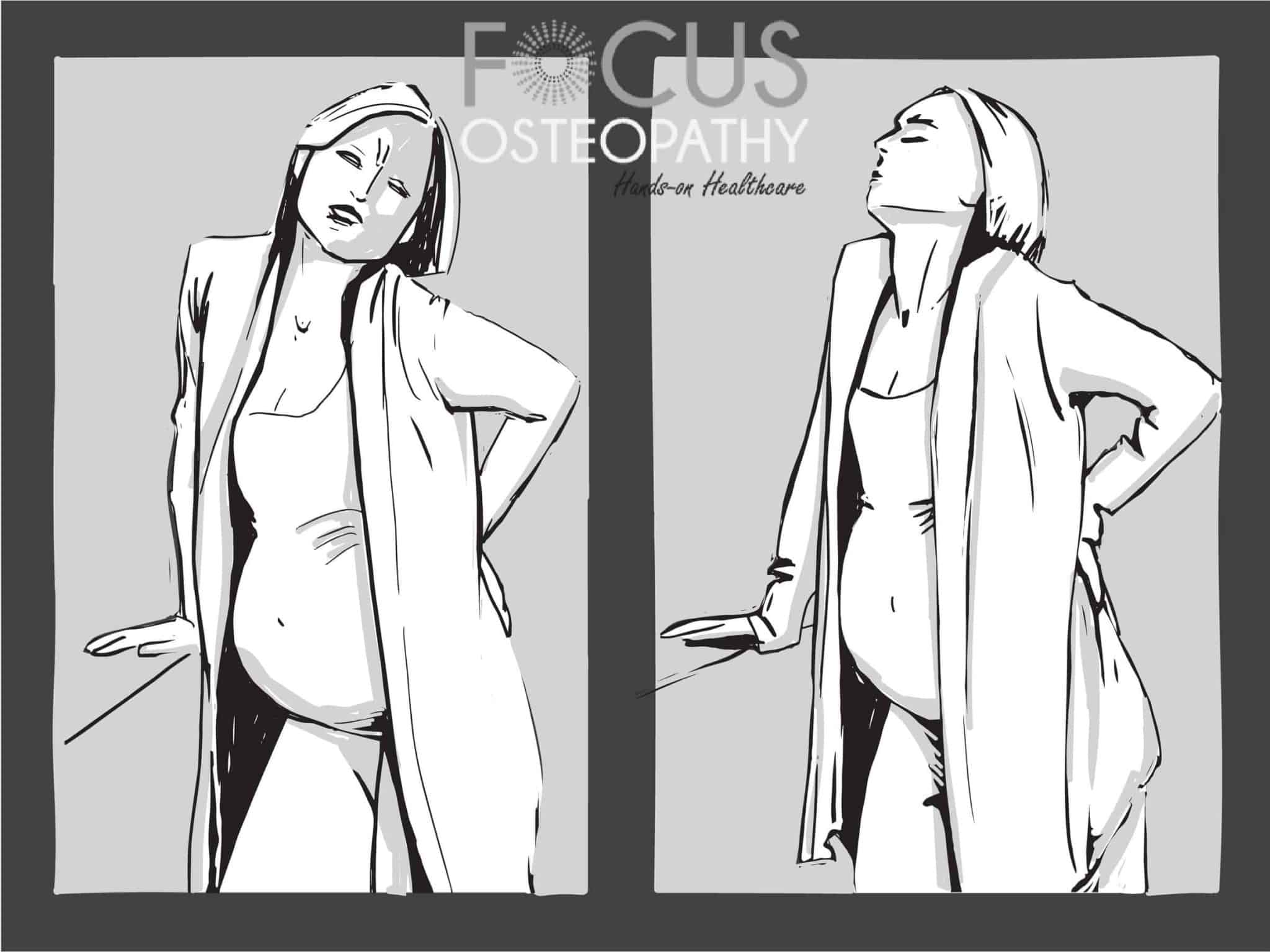
Relieve Joint Pain Caused By Menopause With Our 3 Tips!
Navigating through menopause can often feel like maneuvering through a maze of physical and emotional challenges. One common obstacle that many women face is joint pain. Aching joints can drastically reduce quality of life, making everyday activities a struggle. But rest assured, it’s not an insurmountable problem. In this blog post, we will explore a … Read more