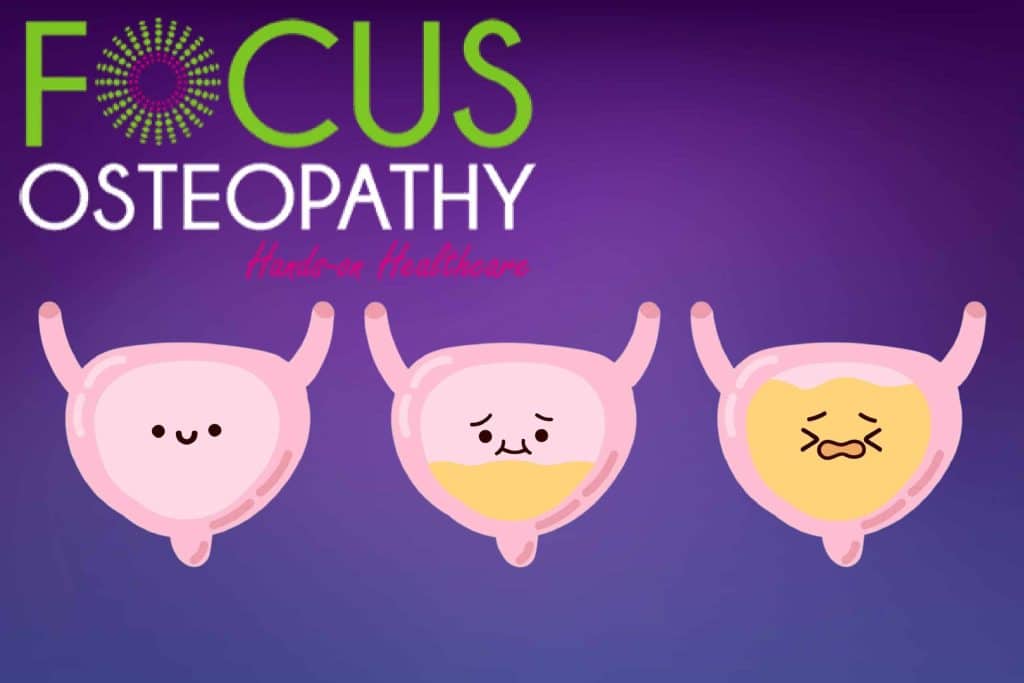
Experiencing urinary problems? Pelvic Floor Dysfunction may be to blame.
When you’re experiencing urinary problems, there’s a high chance that a condition known as ‘Pelvic Floor Dysfunction‘ may be lurking behind the numerous symptoms that are frustrating, exhausting and embarrassing.
More Blogs From Focus Osteopathy

Knee Pain: The Good, The Bad, and the OUCH!

4 Reasons Swimming Is Good For Back Pain
8 Ways Neck Pain Can Disrupt Your Daily Life—and How Osteopathy Can Help
Understanding Back Pain: The Unwanted Companion

Does Massage Therapy Help Sciatica? 4 Things You Must Know

Neck Pain Exercises to Help You Sleep
What is the Pelvic Floor?
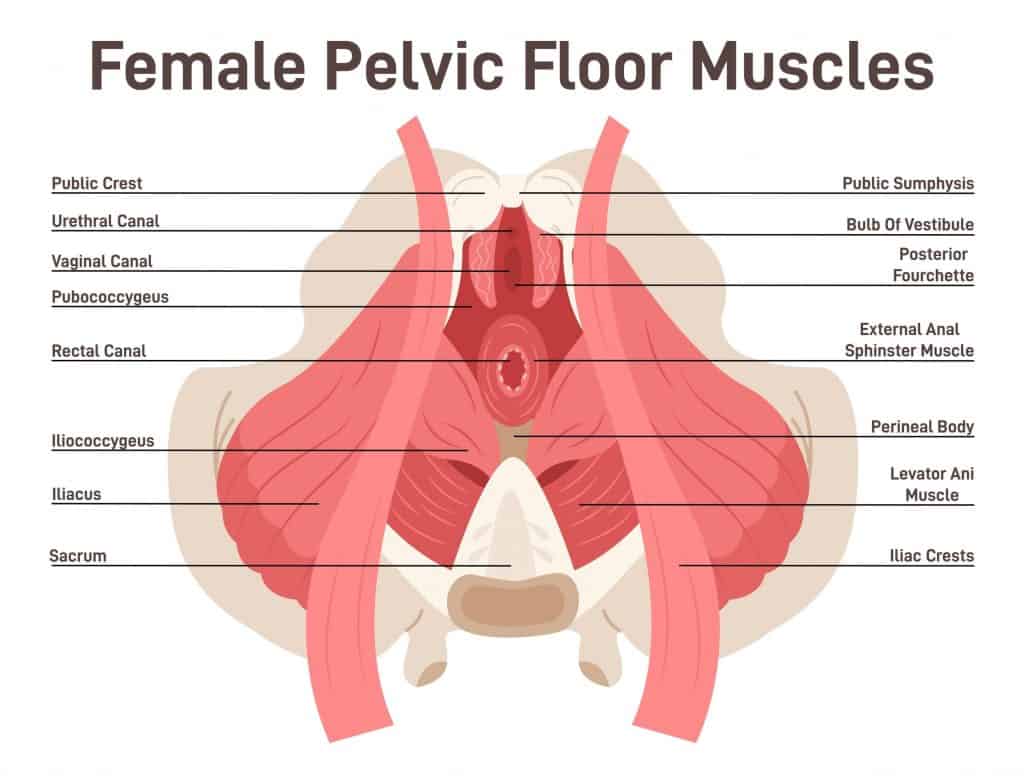
The pelvic floor consists of a group of muscles that form a bowl-shaped hammock, stretching between the pubic bone and the coccyx at the base of the spine. It is a fundamental structure, sitting at a slight tilt and performing several roles including strengthening the abdomen and back, stabilizing the core and controlling urination and defecation.
The pelvic floor holds many internal organs in place, among which are the lower intestine and bladder as well as the prostate in men and the ovaries and uterus in women. During childbirth, the pelvic floor must relax to allow the safe delivery of a baby.
When considering the sheer load of what must be physically supported as well as its many differing functions, the pelvic floor possesses impressive capabilities.
What is Pelvic Floor Dysfunction?
Pelvic Floor Dysfunction (PFD) is an umbrella term that indicates something has gone wrong with the pelvic floor muscles. Many problematic symptoms – including urinary issues – arise in the presence of this condition.
There are two forms of PFD, each dictated by the state of the pelvic floor.
The first form is referred to as hypotonicity (or low muscle tone) and results from weakness in the pelvic floor muscles. In this case, the muscles possess a poor level of contraction, often leading to pelvic organ prolapse (POP) as well as urinary and faecal incontinence and many other symptoms.
The second form of PFD is caused by hypertonicity, where the pelvic floor muscles are tense or tight and cannot fully relax. This can lead to voiding issues with the bladder and bowel as well as pain during intercourse and within the lower back.
PFD is a notable problem among new mothers – the condition registers as the most common complication of childbirth. In rare cases, PFD can be triggered by a sudden injury (e.g., a fall onto the perineum).
PFD can be surprisingly debilitating, often thanks to the interconnected nature of the fascia (connective tissues) within the pelvis. This means that an issue in one area of the pelvic floor has a good chance of impacting another.
For the majority of those with PFD, the problem has built up slowly as a result of multiple concurrent factors, with the condition only manifesting itself symptomatically when a high level of muscle weakness or tightness has developed.
Symptoms of PFD

PFD delivers numerous symptoms, many of which are painful and problematic. Symptoms of PFD develop so gradually that they’re often mistaken as part and parcel of getting older.
As a result, the issue may not be recognized by an individual for many years. Sometimes PFD is detected unexpectedly in a check-up (e.g., ultra-scan) for an entirely different medical matter.
PFD is most commonly associated with urinary incontinence but this is not always the case.
Other possible symptoms include pelvic pain, faecal incontinence, lower back pain, coccyx pain, difficulty sleeping, pain during intercourse, an inability to void or defecate fully, a general feeling of pressure within the pelvis, the urge to urinate frequently, repeated urinary infections and a weak urine stream.
PFD and Urinary Issues in Women
PFD afflicts both genders but not equally. Lifestyle factors such as partaking in high-impact sport, obesity or extended periods of sitting can increase PFD risk in both sexes. However, women are troubled by PFD much more thanks to the various strains and changes that the pelvis undergoes during a woman’s lifetime.
A common cause of PFD in females is childbirth. Over 30% of women experience injury to the pelvic floor during labour. Without adequate muscle training, the pelvic floor is often weak post-partum.
In later life, menopausal hormone changes can encourage PFD to develop. Over half of women over the age of 50 experience a degree of pelvic organ prolapse (POP).
Often, caused by weakness within the pelvic floor, POP allows an organ to shift and this causes issues by putting unexpected pressure elsewhere in the pelvis. Undergoing a hysterectomy will increase the chances of POP and PFD occurring.
On the other hand, significant POP can also be the reason why some women have a hysterectomy.
One of the stand-out symptoms of PFD in women is urinary difficulty. This can take the form of urinary leaks when coughing, sneezing and moving around (urinary incontinence) or difficulty emptying the bladder (urinary retention).
Urinary incontinence is frequently associated with decreasing oestrogen levels while urinary retention is caused by either an obstruction near the bladder or dysfunction of a bladder muscle.

These issues can be caused by POP, changing hormone levels, a tumour or uterine fibroids compressing the urethra or neurological damage that stems from a chronic illness such as diabetes or multiple sclerosis. Occasionally, a retroverted gravid uterus can cause urinary retention post-partum.
The bladder itself can prolapse within the pelvis. When this occurs, it is medically referred to as a cystocele. The fallen bladder then presses against the front vaginal wall, causing a feeling of heaviness. Bladder prolapse can occur solo or in conjunction with uterine or rectal prolapse and this is usually determined by the overall condition of the pelvic floor.
Around a quarter of women will develop PFD but sadly, due to lack of awareness on the condition and the embarrassment that accompanies tackling the problem, only a small proportion actually seek treatment.
Treating PFD and Urinary Issues with Osteopathy

As osteopaths, it is frustrating to know so many women unknowingly develop PFD and then go on to experience its unpleasant side-effects while avoiding assistance thanks to embarrassment.
This is especially true when we know that the condition is easy to diagnose and responsive to the appropriate treatment. PFD cases either disappear or significantly improve with manual therapy and rehabilitation advice, including osteopathy.
Which specific form of PFD has arisen is diagnosed via its symptoms and from which organ the issues originate from.
If you suspect PFD, do not let embarrassment stop you from seeking help. This is important for the longer PFD is left unmanaged, the more treatment is usually needed.
For example, urinary retention is very uncomfortable and, if not addressed, it can be dangerous too. When the bladder cannot empty sufficiently, this can cause renal damage long-term and then both issues require treatment.
To obtain an accurate diagnosis, your osteopath will find it helpful to know your medical background as well as what symptoms you are experiencing. PFD can be caused by other issues so be sure to give as much detail as you can.
50% of people with constipation also have PFD, caused by the constant strain during defecation. By remedying one issue, even if it may seem unrelated, you may also address PFD.
Upon consultation, your osteopath will want to establish what issues, if any, are present within your pelvic floor. You may be asked to breathe, sit, stand and walk within the clinic as moving around helps pinpoint posture issues that could be negatively affecting your pelvic floor.
Your osteopath may also seek to identify muscle trigger points and tight connective tissues that add to your discomfort. Further insight can often be revealed by an internal examination as this allows both the strength and tightness of the muscles in the pelvic floor to be fully evaluated.
Following diagnosis of PFD, your osteopath can develop a rehabilitation plan, which is tailored specifically to remedying the exact form and severity of PFD that you have as well as any associated issues that may also be lingering.
In many cases, simply restoring a higher level of mobility and movement proves enormously beneficial.
This is usually gained through, breath retraining, posture re-training combined with home exercises designed to either strengthen or relax the pelvic floor muscles as required.
In addition, your osteopath may prescribe dietary changes to reduce overall pain and enhance your rehabilitation as you work on the physical elements of your programme.
They may also introduce manual massage or myofascial release into your plan as well as the use of a transcutaneous electrical neural stimulation (TENS) machine or the use of biofeedback sensors.
However your osteopath guides you through rehabilitation therapy, the overall aim will be to combat PFD by restoring healthy function in your pelvic floor.
Your osteopath will also be able to advise on lifestyle habits and either offer direct training or point you in the right direction for other helpful techniques such as meditation, yoga, acupuncture and deep breathing.
Combined, an osteopathic rehabilitation programme can significantly enhance your overall well-being as well as empower you to not let PFD affect your life and lifestyle for good.